Mastering Implant Selection: Choosing Dental Implants for Optimal Osseointegration

Dental implants are widely regarded as one of the most significant advancements in modern dentistry. Since titanium implants were first introduced for intra-oral use in the late 1950s, implantology has emerged as a highly effective and promising solution for the oral rehabilitation of patients who are partially or completely edentulous.
Dr. Brånemark and colleagues first introduced the concept of osseointegration over 45 years ago, which marked the beginning of a new era of research focused on the shapes and materials used for dental implants.
Today, there are approximately 1,300 different implant systems available, each varying in shape, size, material composition, thread design, implant-abutment connections, surface topography, chemistry, wettability, and surface modifications.
Choosing the right dental implant can be a critical decision. Whether you're a dental professional selecting for patients, or a patient making an informed choice, there is an overwhelming number of implant systems on the market.
How do you ensure you're choosing the ideal dental implant that offers a top-notch clinical performance and cost-effectiveness for your practice and patients?
Here are the important points to consider when choosing your ideal dental implant:
1. Evaluate Clinical Research: Look for brands with proven long-term success and strong clinical studies.
2. Check Compatibility: The brand should offer a variety of implant designs, abutment connections, and prosthetic components to fit different cases.
3. Ease of Use: Brands providing user-friendly surgical kits, training, and support can make the process smoother.
4. Aesthetic Focus: Select implants that support healthy soft tissue and offer different aesthetic solutions.
5. Balance Cost vs. Quality: Go for long-term value over initial cost. Some Implant brands provide cost-effective options without compromising quality.
6. Warranty and Availability: Ensure the brand has reliable warranties and is globally available for replacement parts or components.
7. Futureproofing: Choose brands that innovate and integrate with digital workflows to keep your practice up to date.
DESS®CONICAL BLT
DESS® Dental is active in more than 40 countries and offers one of the most comprehensive selections of dental abutments and prosthetic solutions, all designed to be 100% compatible with the top implant systems on the market. DESS® CONICAL BLT is a bone-level tapered Implant designed for full compatibility with Straumann® BL system.
DESS®CONICAL BLT meets all the key criteria for implant selection:
- Preserves crestal bone level and controls micro-gaps.
- Supports both transmucosal and submucosal healing.
- 15-degree internal conical connection with four internal grooves for enhanced stability, reducing the likelihood of screw loosening.
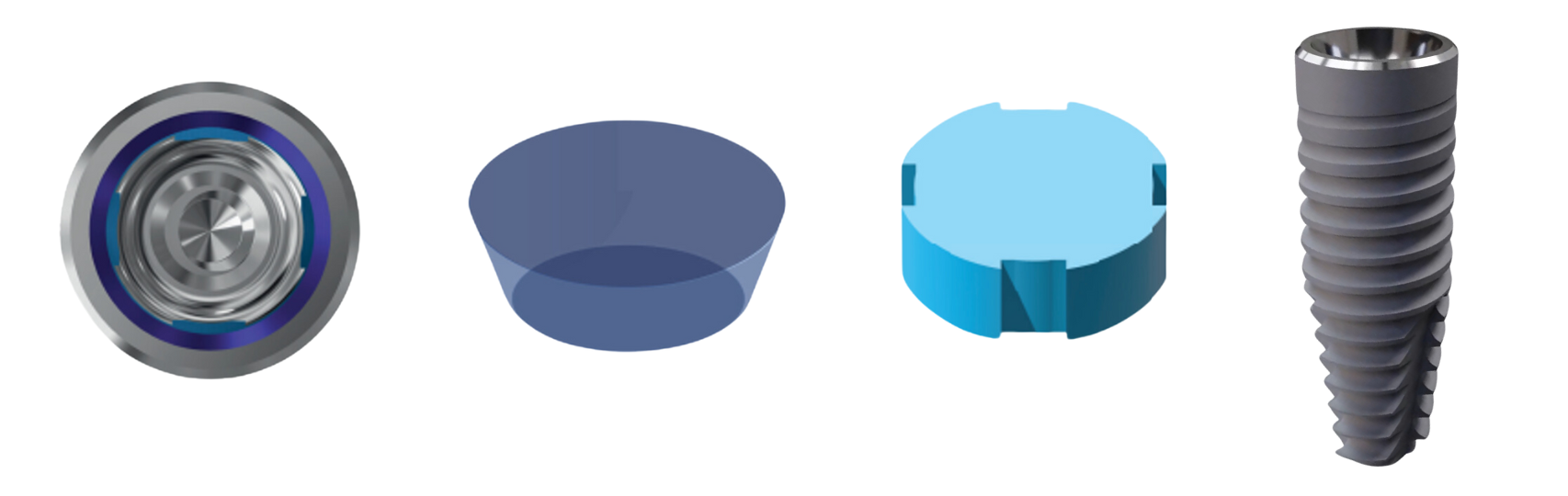 DESS® Osseointegration Surface Technology (OST), adhering to SLA standards
DESS® Osseointegration Surface Technology (OST), adhering to SLA standards
Click here to learn more details about CONICAL BLT’s design
After more than a year of using the DESS® CONICAL BLT Implant, we can confidently say it delivers optimal results. Based on this success, we have decided to lead a dedicated team to conduct a pilot study comparing DESS® Implants with other leading premium brands, including Straumann®, Nobel® Biocare, and Astra Tech Implant SystemTM EV.
This initial study will help us gather valuable preliminary data to assess the performance of these implant systems and inform future, larger-scale research.
ABSTRACT:
Purpose
This study aims to evaluate and compare the marginal bone changes around DESS® (Osseointegration Surface Technology) implants with those observed around three premium implant systems: Straumann (SLA), Astra TechTM (OsseoSpeed), and Nobel Biocare (TiUnite), using Cone Beam Computed Tomography (CBCT) at a 3-month follow-up post-implant placement.
Materials and methods
Study design
Non-randomised prospective cohort study with 40 patients from our clinic, each receiving one of four different types of dental implants in the mandible: DESS®, Straumann®, Astra Tech®, or Nobel® Biocare.
Grouping
Patients were divided into four groups of 10, each corresponding to one implant system. The implants were placed in the mandible region following a standard surgical protocol of the delayed implant placement.
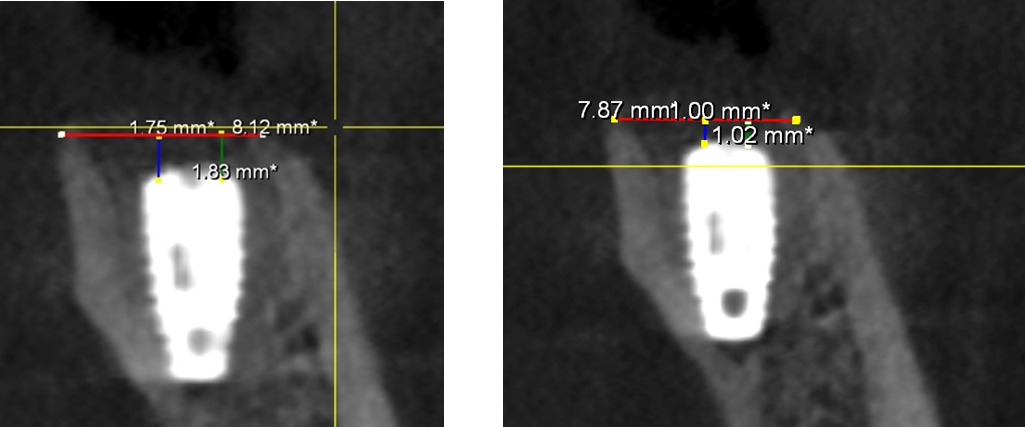
Baseline CBCT imaging was performed immediately after implant placement to measure initial marginal bone levels around the implants. A second CBCT scan was conducted 3 months after the surgery to evaluate changes in marginal bone levels. Marginal bone loss (MBL) was calculated as the difference in bone level measurements between baseline and the 3-month follow-up. Two independent examiners, trained in CBCT analysis, performed the bone measurements to ensure accuracy and reliability.
Results
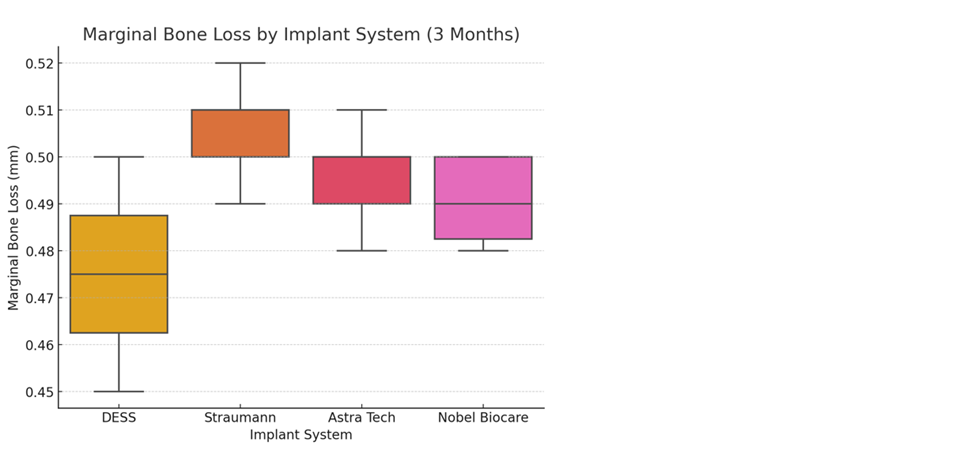
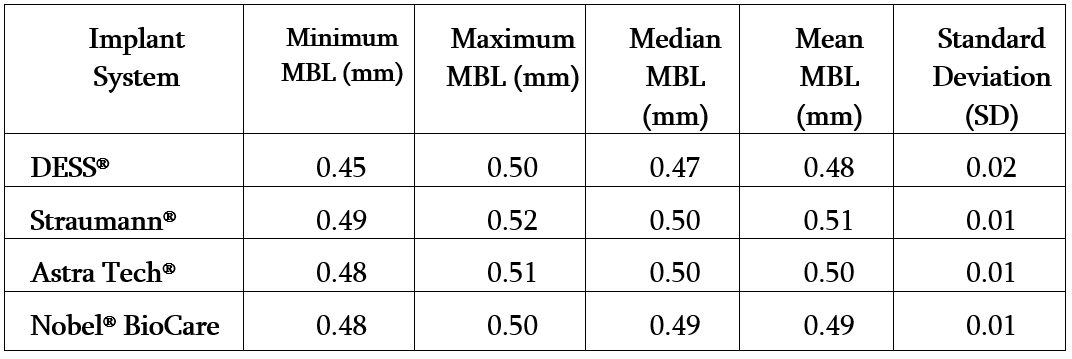
The average marginal bone loss for all implants is approximately 0.5 mm with minor variations between the implant systems.
All groups showed significant bone loss (p < 0.05) from baseline to 3 months, but the differences between the groups were minimal, One-way ANOVA was conducted to compare the mean MBL between DESS®, Straumann®, Astra Tech®, or Nobel® Biocare.
The result showed no statistically significant differences in marginal bone loss between the four groups (p > 0.05), suggesting that all systems exhibited comparable bone loss. The intra-class correlation coefficient (ICC) for the two examiners was 0.95, indicating excellent reliability in bone level measurements.
Conclusion
This preliminary study found no significant differences in marginal bone loss among the four implant systems (DESS®, Straumann®, Astra Tech®, or Nobel® Biocare) after 3 months. The choice between these implants can be based on other clinical factors such as cost, prosthetic compatibility, or patient preference. Additional research with larger sample sizes could help detect subtle differences between these implant systems.
- Figure 1 (A): This CBCT image was taken immediately after implant placement. It shows the initial condition of the crestal bone level.
- Figure 2 (B): This CBCT image was taken 3 months after implant placement. It shows the crestal bone level measurement after 3 months.
Figure: Marginal bone loss after 3 months shows comparable performance across implant systems, with slight variations in mean bone loss.
Table: Summary of Marginal Bone Loss (MBL) Distribution by Implant System